Lion's Mane Mushroom Shows Promise for Neurodevelopment in Children with Autism Spectrum Disorder
- Gauri Khanna

- 3 days ago
- 3 min read
Too long to read? Go for the highlights below.
Bulgarian researchers conducted a 12-month study showing Hericium erinaceus biomass supplementation improved brain wave patterns in 57 children with high-functioning autism spectrum disorder
Quantitative EEG measurements revealed significant reductions in pathological slow-wave brain activity and improvements approaching neurotypical patterns after six and twelve months
The study lacked randomisation and blinding, limiting conclusions, though no adverse effects were reported during the intervention period
Neurodevelopmental disorders present persistent challenges for clinicians, families, and researchers seeking effective interventions. A recent study from Bulgaria's Medical University of Varna examined whether Hericium erinaceus (lion's mane mushroom) biomass supplementation could influence brain development in children diagnosed with autism spectrum disorder and Asperger's syndrome.

Methodology and Participants
The research team, led by Dr Plamen Dimitrov, enrolled 57 children aged 3-6 years with high-functioning autism or Asperger's syndrome, comparing them against 90 neurotypical controls. High-functioning individuals typically demonstrate sufficient language and intellectual abilities to mask social deficits, though they experience challenges including social isolation.
Participants received daily doses of proprietary H. erinaceus biomass tablets (1 gramme for ages 3-4 years, 2 grammes for ages 5-6 years) based on dosing established in previous mild cognitive impairment trials. The biomass comprised whole mushroom material including primordia (early fruiting bodies), cultivated under ISO 22000:2023 food safety certification, distinct from concentrated extracts.

Researchers employed quantitative electroencephalography (qEEG) to track neurological changes at baseline, six months, and twelve months. This technique measures electrical brain activity across different frequency ranges: delta, theta, alpha, and beta waves; each associated with distinct cognitive states and developmental stages.
Brain Wave Pattern Changes
At baseline, children with autism spectrum disorder displayed elevated delta (0.5-4 Hz) and theta (4-8 Hz) wave activity compared to neurotypical children: patterns indicating immature cortical networks and reduced attentional stability. They also showed reduced alpha power (8-12 Hz), suggesting weaker resting-state synchronisation, alongside variable beta activity.
After six months of supplementation, theta power decreased approximately 12-15% in frontal and central brain regions. Alpha activity demonstrated partial normalisation with increased posterior alpha power, supporting improvements in cortical synchronisation. Delta activity showed modest but statistically significant reduction.
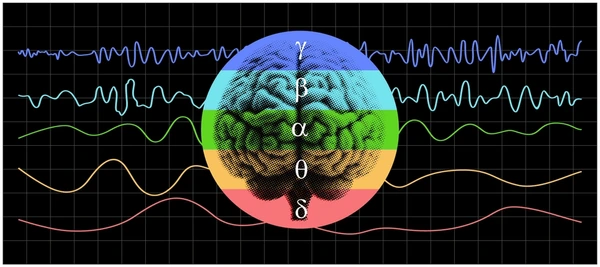
Twelve-month measurements revealed more pronounced shifts. The theta-to-alpha ratio approached values seen in neurotypical controls, suggesting better balance between cortical excitation and inhibition. Delta power decreased further, approaching control norms. Beta1 activity (15-22 Hz) increased moderately in frontal regions, potentially reflecting enhanced executive control.
The treatment worked, causing significant, measurable improvements in brain activity (delta, theta, alpha, and beta frequencies) over the course of the study. Specifically, comparing the start of the study to the six-month and twelve-month check-ups revealed that delta activity experienced the strongest positive change, confirming that the intervention had a substantial effect on the observed brainwave patterns.
Developmental Assessment Results
Beyond brain wave measurements, researchers employed the Developmental Assessment of Young Children (DAYC-2) standardised tool. Cognitive development showed the largest gains: from 30.1% to 64.1% of age-appropriate standards. Speech development improved from 19.3% to 29.1%, adaptive behaviour from 21.8% to 34.3%, and social-emotional development from 24.4% to 35.8%. Physical development, already relatively preserved at 67.9%, increased modestly to 71.3%.
Study Limitations and Mechanistic Considerations
The research lacked randomisation, placebo controls, and blinding: substantial methodological limitations acknowledged by the authors. Without these controls, placebo effects, natural developmental progression, or concurrent interventions cannot be ruled out as contributing factors.
Proposed mechanisms involve H. erinaceus compounds including hericenones and erinacines, which research suggests can cross the blood-brain barrier. The biomass contains polyphenols with antioxidant properties, β-glucans supporting immune modulation, and compounds potentially influencing gut microbiota composition. Studies indicate the mushroom may increase anti-inflammatory mediator lipoxin A4 and modulate inflammatory pathways, though translating preclinical findings to clinical outcomes requires caution.
No adverse effects were reported during the twelve-month intervention period. All 57 participants completed the study without withdrawal due to side effects or non-compliance.
The findings warrant further investigation through properly controlled trials with larger sample sizes, longer follow-up periods, and multimodal outcome measures combining neuroimaging, behavioural assessments, and biomarker analysis. Until such evidence emerges, H. erinaceus supplementation for neurodevelopmental disorders remains an interesting hypothesis requiring rigorous validation.




